MITRAL STENOSIS by PAWAN BHASIN Roll no. 124
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here, we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
May 28, 2020
CASE OF A 55 YEAR OLD FEMALE WITH HEART FAILURE
Written by : PAWANBHASIN
Final MBBS- IV part II
Roll number : 124
Given case data available at this link : https://himabindu5.blogspot.com/2020/05/hello-everyone.html
According to the data provided to me, the analysis made by me is as follows:
Age : 55 years , Sex - female, Occupation - agricultural labourer(works in paddy fields)
Chief complaints:
Patient came with the chief complaint of :
Shortness of breath(since 3 months)
Palpitations(since 2 months)
Chest pain
Swelling of legs upto ankle(since 1 week)
History elaborated:
i) Shortness of breath:
Onset - sudden
Duration- 5 years and increased in intensity in the last 3 months
Progression- gradually progressive (she is unable to carry out her daily chores apart from household activities thus making her Dyspnea grade -III according to NYHA classification.)
Associated complaints -
Orthopnea- since last 3 months, 1-2 episodes per week but in the last 10 days, every night 1 episode.
Paroxysmal Nocturnal Dyspnea
Wheezing
This indicates it could be a cardiac problem or respiratory problem.
ii) Palpitations:
Character- Pounding which indicates -
High output states such as anemia, beri-beri, thyrotoxicosis
Structural abnormalities such as cardiomegaly, Left ventricular failure
iii) Chest pain:
Onset - sudden
Duration - 2 months
Site - more on left side
Radiation - non radiating
iv) Swelling of both the legs upto ankles(Bilateral pedal edema):
Onset- sudden
Duration-1 week
Associated complaints- Oliguria (which relieved on medication)
This indicates it could be a cardiac problem or renal problem.
As there is no periorbital edema which is characteristic of Renal failure, we can rule out primary renal cause. This might be secondary to cardiac problem.
Past history: Had similar complaints 5 years back. She had a sudden onset of fever with cough which lasted for 5 days and got relieved on medication. It could have been Rheumatic fever. But there was no documentation of Rheumatic fever or the treatment taken for it.
From the provided history :
PND,Orthopnea,Wheeze are suggestive of respiratory problem but there is No cough,No hemoptysis ,No expectorant so i rule out primary Respiratory involvement but could be secondary to Right heart Failure
PND,Orthopnea,Palpitations,Chest pain,Pedal edema,Oliguria,Shortness of breath favor cardiac cause. so on the basis of this I am of the opinion that the primary cause is in the Heart. Now it could be Left heart failure or Right heart failure. On the basis of symptoms,it is more suggestive of primary Left Heart Failure causing secondary Right heart failure.?
Examination findings:
1. Respiratory system:
Wheezing in right side (could be because of Heart Failure) , Coarse crepitations in right side (indicating Pulmonary oedema)This indicates that there could be Left Heart Failure.
2. CVS:
i) Peripheral Examination-
a) Pulse: Normal rate, Irregularly irregular rhythm with no apex pulse deficit, feeble.
This might be due to the following causes:
Atrial Fibrillation(But there is no apex pulse deficit)
Atrial Tachycardia
Feeble pulse could be because of heart failure, shock, mitral stenosis
b) JVP: Increase in JVP with large 'a' waves. Causes for this are: Any condition in which more force is required for blood to enter into Right ventricle from Right atrium.
Tricuspid stenosis
Right Ventricular hypertrophy
Right Atrial Tumour
Pulmonary hypertension
ii) Examination of the precordium:
a) Inspection:
Slight kyphosis of the back
b) Palpation:
Apex beat is displaced downwards and outwards (indicating chronic Left Ventricular failure, could be because of the kyphosis also).
Parasternal heave (indicates Right ventricular hypertrophy)
c) Auscultation:
Loud S1 in mitral area (could be because of mitral stenosis).
Splitting of S2 in pulmonary area with loud P2 (could be because of Pulmonary artery hypertension).
After examination, I am of the opinion that it could be a case of Left heart failure. The possible causes for it in this patient could be:
Mitral stenosis
Coronary Artery Disease
Cardiomyopathy
Anemia
Left Atrial myxoma
Investigations done already:
CBP- showed Microcytic hypochromic anemia with neutrophilia (indicates Chronic heart failure)
RFT-
Elevated blood urea
Elevated uric acid
Elevated Calcium
Elevated Phosphorus
Patient also gives a history of oliguria.
The above indicate that there is a kidney shutdown due to decreased blood availability that might be due to a chronic heart failure
LFT-
Elevated total bilrubin levels.
Heart Failure with reduced ejection fraction(HFrEF) causes two times increase in bilirubin levels than HFpEF.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3331650/
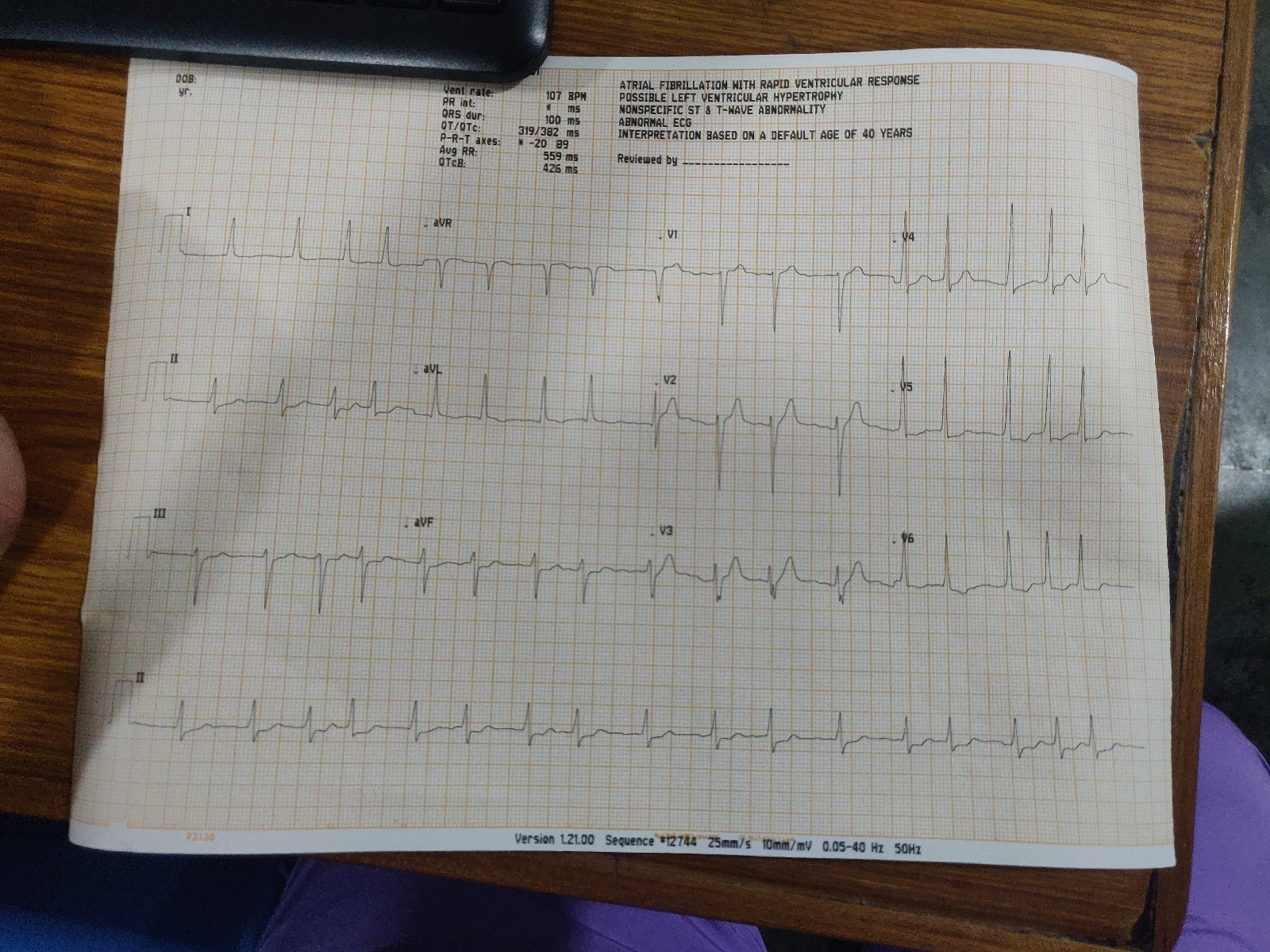
ECG-
Absent p waves (Indicates atrial fibrillisation).
Right axis deviation (indicates Right ventricular hypertrophy).
ST elevation in V4,V5,aVR (indicating Lateral wall MI). Because of this, troponin levels were also investigated which was negative.
Chest X ray (PA view)-
Cardiomegaly-Hypertrophy of left ventricle, right atrium and right ventricle.
Mitalisation is seen i.e straightening of left border of heart and is due to-
i) Aortic Knuckle- Small
ii) Convexity due to dilated pulmonary artery (Pulmonary Hypertension)
iii) Left atrial appendage becomes prominent and produces a convexity.
iv) Double contour of right border of heart
v) Evidence of pulmonary hypertension-
Dilated pulmonary arteries
2D ECHO-
Fish mouth appearance of the mitral valve (suggestive of Mitral stenosis)-
Calcified mitral valve
Thickened immobile cusps
Reduced valve area
After investigations I can confirm that this is a case of Left Heart Failure due to Mitral Stenosis.
Risk factors in this patient:
Age- 55 years
Sex- Female (greater risk for mitral stenosis)
Had a previous similar history
Anatomical location of the root cause is in the mitral valve. The chordae tendinae and leaflets gets shortened to produce stenosis.
PATHOPHYSIOLOGY responsible is :
Various etiologies responsible for mitral stenosis in this particular patient:
Rheumatic Fever (but there is no documentation)
Ageing (causing calcification of the valve)
Congenital mitral stenosis (secondary to parachute mitral valve or Lutembacher's syndrome).
Complications of Mitral stenosis in this patient are:
Left Heart failure
Pulmonary artery hypertension
Atrial Fibrillation (but there is no apex pulse deficit)
Renal failure (because of the LHF)
Addtional Investigations and Examinations required are:
Doppler study - To record the pressure gradient across mitral valve and pulmonary artery systolic pressure.
Cardiac catheterisation- To determine the hemodynamic status of the patient
Characteristic murmur of Mitral Stenosis - mid diastolic rumbling murmur
Opening snap might be present.
Transoesophageal echocardiography
TFT (Thyroid Function Tests) should be done.
To diagnose rheumatic carditis, ASO titres are checked (which will be raised).
Cardiac MRI - Gold standard to diagnose Heart Failure
BNP levels (Brain Natriuretic Peptide): can help in the prognosis oh heart failure
Provisional diagnosis:
Mitral Stenosis with heart failure
Treatment plan:
MEDICAL MANAGEMENT
Pharmacological:
- Tab. Diuretics (Lasix - for Pulmonary Edema)
- Tab. Budecort (For shortness of breath)
- Anti-Coagulants with warfarin orally (To prevent Thrombi formation)
- Antibiotics (To prevent infections)
- Fluid and salt restriction
- Tab. Pantop
- Additional drugs: can be givenSacubitril/Valsartan (Entresto)IvabradineOmecativ mecarbil (new cardiac myosin activator)Tolvaptan (oral vasopressin type 2 receptor antagonist) Advantage of this over loop diuretics is causes diuresis without any electrolyte imbalance.
Non pharmacological:
Diet and nutrition mainly salt and fluid restriction.
Adequate rest and Physical activity.
Improve symptom recognition and self care behaviour
Yoga, meditation may reduce the anxiety in patients and can also improve the breathing
Continuous Positive Airway Pressure (CPAP) to improve daily functional activity and quality of life.
Adequate disease managaement and follow up of the patient with Heart Failure can reduce readmission rates.
Surgical Management:
(If not improved through the Medical Management)
- Valve replacement(Prosthetic valves) or
- Open volvotomy
PREVENTION
Rheumatic Heart Disease:
Primary- Penicillin prophylaxis can prevent an attack of rheumatic fever in a patient presenting with acute pharyngitis caused by Group A streptococcal infection.
Secondary- To prevent further attacks by Group A beta hemolytic streptococcus in a patient who had a previous rheumatic fever.
2. Pneumococcal and Influenza vaccination may reduce the incidence of respiratory infections that may worsen Heart Failure.
https://www.ecrjournal.com/articles/non-pharmacological-management
References :
1) Hutchison’s clinical methods
2) Harrison’s principles of internal medicine
3)Clinical methods of medicine by Arup Kumar Kundu
4) Davidson’s principles and practice of medicine
5)https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3331650/
6) https://www.mayoclinic.org/diseases-conditions/mitral-valve-stenosis/symptoms-causes/syc-20353159


Comments
Post a Comment